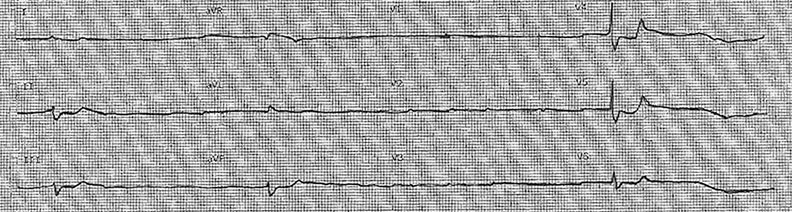
This is a 65 y/o WM who has a history of paroxysmal atrial fibrillation and CHF presents via EMS with lethargy, weakness and intermittent syncope. The family found a mostly empty bottle of digoxin in his apartment. Vitals: 24 75/25 6 99% RA. You are handed the following 12 lead ECG by EMS:
The decision is made to begin transcutaneous pacing the patient. The pads are placed and the pacing mode is selected. You are convinced you feel a pulse, and the following ECG strip is obtained:

But the patient remains unconscious. You obtain the following ultrasound. What is the cause of the patient’s continued poor clinical status?
Answer: Poor pacing capture
This patient presents with suspected digoxin toxicity and symptomatic third degree heart block, so transcutaneous pacing (TCP) was instituted immediately. Although a pulse was felt during pacing, the ECG strip was equivocal for capture and the patient did not show any clinical improvement. This echo confirmed our suspicion that the patient did not have electromechanical capture (EMC).
- While cardiac pacing a patient with heart block, it is imperative to confirm EMC.
- It can be difficult to tell if the patient has attained EMC simply by looking at an ECG strip while being transcutaneously paced, as ECG machines do not have the proper electronic dampening for cutaneous pacer spikes (use a regular monitor strip and look for a wide complex QRS with a trailing t-wave).1
- Skeletal muscle stimulation can often result in the sensation that the patient has a pulse, yielding a false positive. Poor pulse volume while pacing can result in a false negative pulse.
- Bedside echocardiography can easily tell you if you have obtained EMC.
- It is simple to implement transcutaneous pacing with bedside echo:This clip demonstrates what you will see as the current is increased and EMC is obtained:
- Place pacer pads on the patient (ant/posterior preferred1)
- Set the pacer/defibrillator to pacing mode
- Set a rate of 60-70
- Obtain an echo view of the LV
- While watching for increased LV rate, increase current every few seconds in 5-10 mA increments until EMC is obtained
- Once EMC is obtained, increase the current by 25%2
- Provide analgesia/anxiolysis to the patient if conscious
- This clip demonstrates what you will see as the current is increased and EMC is obtained:
- To confirm 100% capture, m-mode can be utilized to measure the heart rate. If it matches the rate set on the pacemaker, full capture is confirmed.3
- Physiologic stress such as worsening acidosis or hypoxia can increase the pacing current capture threshold, so these patients need constant monitoring to ensure consistent capture.
- Remember to consider floating a transvenous (TV) pacer wire if the expected clinical course includes prolonged pacing, as TCP can be quite uncomfortable for the patient and result in cutaneous burns.
- Ultrasound has been shown to be effective at identifying RV pacer wire position.4,5 This clip demonstrates a TV pacer wire in the RV, with the tip at the apex:
- The use of ultrasound contrast to fill the TV pacer balloon has been shown to improve TV pacer visualization for even more precise placement.6
- Roberts JR, Hedges JR. Clinical Procedures in Emergency Medicine. Elsevier Health Sciences; 2013.Tam MM. Ultrasound for transcutaneous pacing: documentation, usage, and definition. Am J Emerg Med. 2005;23(2):197-8. [ACEP Bookstore]
- Tintinalli J, Stapczynski J, Ma OJ et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, Seventh Edition (Book and DVD). Mcgraw-hill; 2010. [ACEP Bookstore]
- Blanco P, Nomura JT. An atypical misplacement of a temporary pacing catheter diagnosed and resolved by ultrasound. Am J Emerg Med. 2014; [pubmed]
- Aguilera PA, Durham BA, Riley DA. Emergency transvenous cardiac pacing placement using ultrasound guidance. Ann Emerg Med. 2000;36(3):224-7. [pubmed]
- Kaemmerer H, Kochs M, Hombach V. Ultrasound-guided positioning of temporary pacing catheters and pulmonary artery catheters after echogenic marking. Clin Intensive Care. 1993;4(1):4-7. [pubmed]


