Diagnosis: Severe Pulmonary Hypertension
This echocardiogram demonstrates profound RV dilation, suspected to be secondary to severe pulmonary hypertension. Despite FiO2 of 100% sats were in the 50’s so inhaled nitric oxide was started to empirically treat the pulmonary hypertension. The patient’s oxygen saturation jumped to 100% after just a few minutes of this treatment regimen. His FiO2 was slowly weaned down before he was transferred to see a pulmonary hypertension specialist.
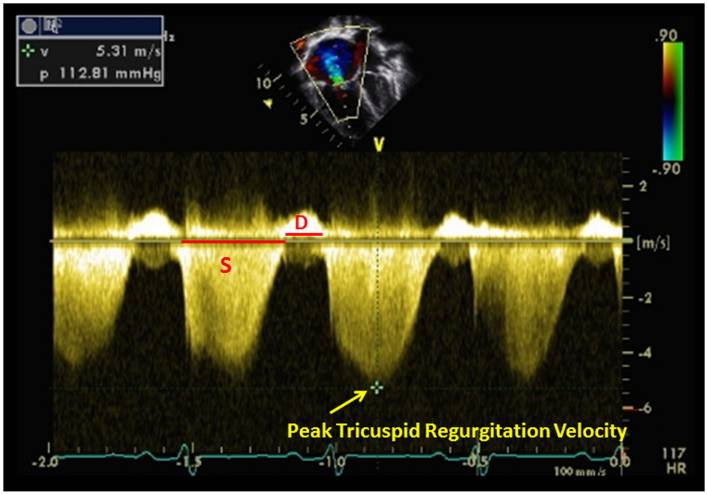
- Signs of pulmonary hypertension on bedside echo include an RV:LV ratio > 1:1 on the apical view, a D-shaped left ventricle on the PSAX view (flattening of the interventricular septum on apical/PLAX view), and tricuspid regurgitation (TR).

- The IVC inspiratory collapse percentage can help estimate right atrial pressure (RAP, same as central venous pressure) in the infant population, just as it can in adults.1 Remember that the 50% IVC collapse cutoff is reliable only in the spontaneously breathing patient. The <50% IVC collapse in this patient predicts a RAP of ~15 mmHg. Absolute IVC size varies in children, so it is not a reliable indicator of RAP.
- To estimate right ventricular systolic pressure (RVSP, same as pulmonary artery systolic pressure assuming no obstruction between the PA and RV) you must add your estimated RAP to the pressure gradient you obtain by measuring the maximal TR jet. Here is a handy RVSP calculator to do the hard math for you. An RVSP of < 30 mmHg is normal, although a cutoff of 40 mmHg is considered normal in the obese and elderly.2
- In the pediatric population, the most common causes of pulmonary hypertension are idiopathic and congenital heart defects.3
- Pediatric patients with acute respiratory distress syndrome have been shown to respond to inhaled nitric oxide as empiric treatment.4,5 This treatment is especially useful in patients with pulmonary hypertension.
- Jone PN, Ivy DD. Echocardiography in Pediatric Pulmonary Hypertension. Front Pediatr. 2014;2:124. [PDF]
- McQuillan BM, Picard MH. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001;104(23):2797-802. [PDF]
- Beghetti M, Berger RMF. The challenges in paediatric pulmonary arterial hypertension. European Respiratory Review. 2014;23(134):498–504. [PDF]
- Dellinger RP, Zimmerman JL, Taylor RW, Straube RC, Hauser Dl, Criner GJ, Davis K, Hyers TM, Papdakos P. Effects of inhaled nitric oxide in patients with acute respiratory distress syndrome: results of a randomized phase II trial. Crit Care Med. 1998;26:15–23. [PubMed]
- Troncy E, Collet JP, Shapiro S, Guimond JG, Blair L, Ducruet T, Francoeur M, Charbonneau M, Blaise G. Inhaled nitric oxide in acute respiratory distress syndrome: a pilot randomized controlled study. Am J Respir Crit Care Med. 1998;157:1483–1488. [PubMed]



