61 yo female with no previous medical history presenting with nausea, vomiting and epigastric pain that began approximately 4 hours after eating at a mexican restaurant. Vital signs showed sinus tachycardia and mild hypoxia with the patient sating 92% on room air. Abdominal ultrasound was performed, identifying a normal gallbladder. However, due to the patients age and abnormal vital signs, an echo was performed immediately after the gallbladder ultrasound and identified the following:

Answer: Regional Wall Motion Abnormality due to LAD occlusion
Bedside echo performed identified global hypokinesis, with wall motion abnormalities worse in the septal and apical segments. Thoracic ultrasound shows bilateral b-lines consistent with pulmonary edema. These findings were confirmed by an complete echocardiography performed by the cardiology department a few hours later.
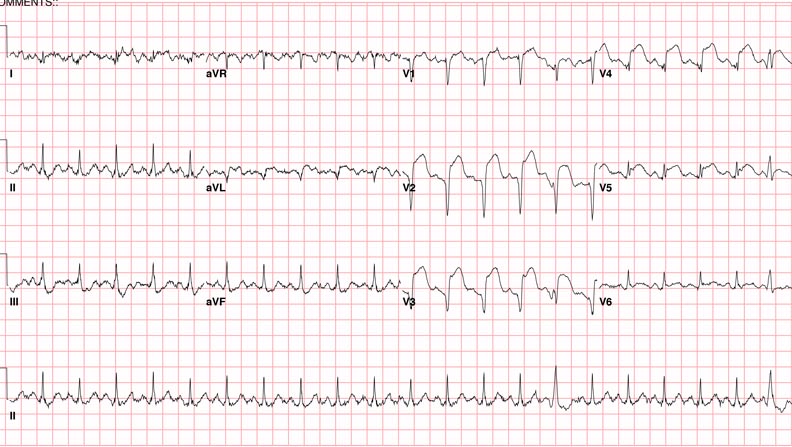
An EKG was then performed that showed diffuse anterior-lateral STEMI with depressions in the inferior leads, with a troponin of 12.3.
The patient was then taken emergently to cath lab and found to have a 100% osital LAD lesion that was successfully stented with some difficulty.
- Ostial lesions are defined as arising within 3 mm of the vessel origin. These lesions have the reputation of being associated with lower successful PCI and higher complication rates when compared to non-ostial lesions.1
- Various views can be used to identify regional wall motion abnormalities (RWMA), which can be seen as hypokinesis in relation to adjacent walls.
- When evaluating the heart for RWMA, it has been recommended to divide the heart into 17 segments for assessment of the myocardium and the left ventricular cavity2, however a more simplified method may be more ideal of the point-of-care evaluation of a patient with suspected RWMA.
- A more simplified method has been suggested by Lang et al2 which focuses on identification of the distribution of the right coronary artery (RCA), left anterior descending artery (LAD) and the circumflex artery (CX).
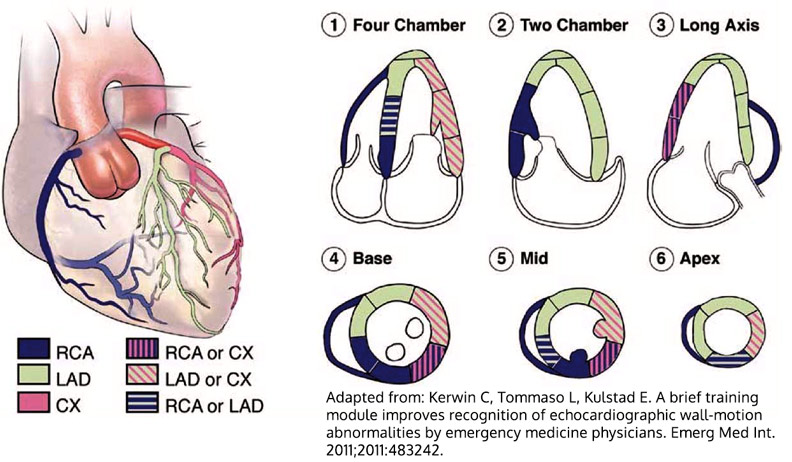
- Emergency physicians can be trained to identify these lesions with good accuracy. A study by Kerwin et al found that after a brief, 30 minute training module, median percentages correct improved from 67% to 87% when reviewing pre-recorded clips.3
- Jokhi P, Curzen N. Percutaneous coronary intervention of ostial lesions. EuroIntervention. 2009;5:(4)511-4. [pubmed]
- Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:(12)1440-63. [pubmed]
- Kerwin C, Tommaso L, Kulstad E. A brief training module improves recognition of echocardiographic wall-motion abnormalities by emergency medicine physicians. Emerg Med Int. 2011;2011:483242. [pubmed]





