A 73 year old female presents with sudden onset of midsternal chest pain and shortness of breath. The pain is worse with deep respiration and does not radiate. The patient appears to be in severe pain and is diaphoretic. BP 82/45 P 74 O2 sat 95% RA.

Answer: rupturing thoracic aortic aneurysm
This apical bedside echocardiogram demonstrates a normal appearing left ventricular ejection fraction and no evidence of pericardial effusion. Also noted is a large amount of mid-echogenic material surrounding the descending aorta. This large volume of material is most consistent with mural thrombus in a descending thoracic aneurysm. Additionally it is evident that the aneurysmal sac partially compresses the left atrium (LA), potentially limiting LA filling.
- Although literature is scarce on using bedside transthoracic echocardiography (TTE) to specifically diagnose thoracic aneurysm, one would expect the sensitivity to be similar to that of TTE for aortic dissection.
- TTE has a reported sensitivity for thoracic dissection of 59% to 83% and specificity is 63% to 93%. The sensitivity for Type A dissections (78% to 100%) is higher than type B dissections (only 31% to 55%).1,2,3
- With this in mind, bedside ultrasound should be viewed as being able to rule in thoracic aneurysm when there is good visualization of a dilated aorta, but its poor sensitivity means that TTE should not be relied on to rule out an acute thoracic aortic syndrome.

- In the undifferentiated patient with chest pain and hypotension, secondary signs of thoracic aneurysm or dissection on TTE should raise suspicion of an acute aortic syndrome: pericardial effusion, aortic insufficiency/regurgitation and wall motion abnormalities.
- Transesophageal echocardiography, on the other hand, has been shown to have a sensitivity approaching 99% and a specificity of around 90%.4,5,6,7
- A thoracic aorta measuring 4-5 cm is considered dilated, while one measuring > 5 cm is considered aneurysmal.8 Remember to include any thrombus in the measurement of the aneurysm.
- CTA is the imaging modality of choice to rule in aneurysm and identify signs of active extravasation and active rupture. Above is the CTA from our patient.
- For TTE, measurement of the aortic root on the parasternal long axis view can help to identify type A aneurysms, upper limit of normal here is 4cm.

- To view the aortic arch, it is useful to obtain a sternal notch view. Having the patient's head extended off the end of the bed may aid in positioning for this view.
- The descending thoracic aorta can be visualized in short axis from the parasternal long axis and the apical views, as in this case. From a parasternal long axis position, rotation of the probe slowly clockwise 45 degrees will allow visualization of the descending aorta in long axis.
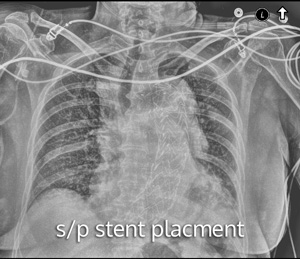 The patient in this case received emergent vascular surgery consultation, where she received the prompt placement of a stent in the descending aortic aneurysm. Her vital signs stabilized and she was discharged from the hospital a few days later.
The patient in this case received emergent vascular surgery consultation, where she received the prompt placement of a stent in the descending aortic aneurysm. Her vital signs stabilized and she was discharged from the hospital a few days later.
 If you like the ultrasound education you get from UOTW, you will absolutely love CastleFest, a world class ultrasound event held in April. Whether you're an ultrasound novice or want to hone your experienced skills, come eat, drink and learn with the best educators in the field: Dawson, Mallin, Weingart, Mallemat, and more. Oh, and I'll be there too. Register now.
If you like the ultrasound education you get from UOTW, you will absolutely love CastleFest, a world class ultrasound event held in April. Whether you're an ultrasound novice or want to hone your experienced skills, come eat, drink and learn with the best educators in the field: Dawson, Mallin, Weingart, Mallemat, and more. Oh, and I'll be there too. Register now.
- Granato JE, Dee P, Gibson RS. Utility of two-dimensional echocardiography in suspected ascending aortic dissection. The American journal of cardiology. 56(1):123-9. 1985. [pubmed]
- Iliceto S, Antonelli G, Biasco G, Rizzon P. Two-dimensional echocardiographic evaluation of aneurysms of the descending thoracic aorta. Circulation. 66(5):1045-1049. 1982. [article]
- Victor MF, Mintz GS, Kotler MN, Wilson AR, Segal BL. Two dimensional echocardiographic diagnosis of aortic dissection. The American journal of cardiology. 48(6):1155-9. 1981. [pubmed]
- Goldstein SA, Lindsay J, Vasan R. The diagnosis of thoracic aortic dissection by noninvasive imaging procedures. The New England journal of medicine. 328(22):1637-8. 1993. [pubmed]
- Moore AG, Eagle KA, Bruckman D. Choice of computed tomography, transesophageal echocardiography, magnetic resonance imaging, and aortography in acute aortic dissection: International Registry of Acute Aortic Dissection (IRAD). The American journal of cardiology. 89(10):1235-8. 2002. [pubmed]
- Erbel R. Diagnosis and management of aortic dissection Task Force on Aortic Dissection, European Society of Cardiology. European Heart Journal. 22(18):1642-1681. 2001. [article]
- Sommer T, Fehske W, Holzknecht N. Aortic dissection: a comparative study of diagnosis with spiral CT, multiplanar transesophageal echocardiography, and MR imaging. Radiology. 199(2):347-52. 1996. [pubmed]
- Webb WR, Higgins CB. Thoracic Imaging, Pulmonary and Cardiovascular Radiology. Lippincott Williams & Wilkins; 2010.




