This 56 year old smoker with a history of HIV and anal cancer presents with complaints of 1 month of gradual onset severe shortness of breath, much worse for the past week. Vitals: 82/46 130 98.6F 30 75%RA.



Answer: Severe Chronic Pulmonary Hypertension
This echocardiogram demonstrates a severely dilated right ventricle with bowing of the septum into the left ventricle. The right ventricular (RV) free wall does appear thickened, but is hypokinetic. There is evidence of apical RV contractility, so there is a McConnell’s sign noted. TR jet velocity is very high. The ECG here demonstrates signs of significant RV strain: a RBBB with inverted T-waves in II/III/aVf and V1-V4. CTA of the chest was performed and demonstrated no evidence of pulmonary embolism.
- As we have mentioned here before, the initial Mcconnell Sign study showed a 94% specificity for PE, but subsequent studies have shown that it can be seen in acute RV infarct and up to 17% or patients with chronic pulmonary hypertension.1,2,3 It should therefore not be viewed as definitive proof of pulmonary embolism. Other than clot in transit, there are no pathognomonic signs of pulmonary embolism on bedside echo.
- A bedside ultrasound is a test. As such, the usual Bayesian statistics apply, and any scan should be viewed through the lens of the patient’s clinical context. This patient’s presentation, while dramatic, was not typical of a massive pulmonary embolism. Given the fact that ultrasound is not specific for this diagnosis, our post test probability for pulmonary embolism is not high. In this situation, a gold standard test (CTA chest) is needed before instituting an invasive treatment such as thombolysis.
- An RV wall thickness of 5 mm or larger as well as a tricuspid regurgitant jet velocity > 370 cm/s are more suggestive of chronic pulmonary hypertension rather than an acute event.4 This results from the chronic RV adaptation to high afterload: RV hypertrophy. In acute pulmonary hypertension, the sudden increased afterload thins out the RV wall as it is unable to squeeze against such a high load. This much weaker RV cannot generate such high RV systolic pressures, resulting in a slower TR jet than seen with chronic PH.
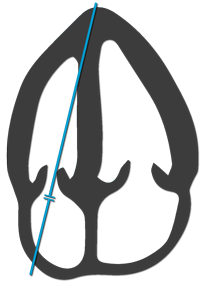
- Pulmonary hypertension can be diagnosed by measuring the peak TR jet velocity (placing the continuous wave doppler as in the diagram above) and looking at IVC diameter / respiratory-phasic changes.
| IVC | Inspiratory Δ | RA Pressure |
| Normal (≤2.1 cm) | >50% | 3 mmHg |
| Normal (≤2.1 cm) | ≤50% | 8 mmHg |
| Dilated (>2.1 cm) | ≤50% | 15 mmHg |
- Once these measurements are made, use this calculator based on the Modified Bernoulli Equation to estimate the RV systolic pressure (RVSP). RVSP is the same as PA systolic pressure, assuming no pulmonic stenosis.5 One study found that an RVSP cutoff of 39 mmHg was 87% sensitive and 81% specific for pulmonary hypertension.6 Unfortunately, RVSP does not correlate well with the severity of PH (especially in severe disease) and so it should not be used to stage the degree of disease.7,8
 If you like the ultrasound education you get from UOTW, you will absolutely love CastleFest, a world class ultrasound event held in April. Whether you’re an ultrasound novice or want to hone your experienced skills, come eat, drink and learn with the best educators in the field: Dawson, Mallin, Weingart, Mallemat, and more. Oh, and I’ll be there too. Register now.
If you like the ultrasound education you get from UOTW, you will absolutely love CastleFest, a world class ultrasound event held in April. Whether you’re an ultrasound novice or want to hone your experienced skills, come eat, drink and learn with the best educators in the field: Dawson, Mallin, Weingart, Mallemat, and more. Oh, and I’ll be there too. Register now.
- McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. The American journal of cardiology. 78(4):469-73. 1996. [pubmed]
- Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005;6(1):11-4. [PDF]
- López-Candales A, Edelman K. Right ventricular outflow tract systolic excursion: a distinguishing echocardiographic finding in acute pulmonary embolism. Echocardiography (Mount Kisco, N.Y.). 30(6):649-57. 2013. [pubmed]
- Wood KE. Major Pulmonary Embolism . Chest. 121(3):877-. 2002. [article]
- Otto CM. Textbook of Clinical Echocardiography, Expert Consult – Online and Print. Elsevier Health Sciences; 2013. [Google Book]
- Bech-Hanssen O, Karason K, Rundqvist B, Bollano E, Lindgren F, Selimovic N. Can pulmonary hypertension and increased pulmonary vascular resistance be ruled in and ruled out by echocardiography? Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 26(5):469-78. 2013. [pubmed]
- Rich JD, Shah SJ, Swamy RS, Kamp A, Rich S. Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension: implications for clinical practice. Chest. 139(5):988-93. 2011. [pubmed]
- Farber HW, Foreman AJ, Miller DP, McGoon MD. REVEAL Registry: correlation of right heart catheterization and echocardiography in patients with pulmonary arterial hypertension. Congestive heart failure (Greenwich, Conn.). 17(2):56-64. 2011. [pubmed]




